.
Breast cancer: Symptoms, risk factors, and treatment
By Christian Nordqvist
An early diagnosis of breast cancer increases the chance of recovery.
Breast cancer is the most common invasive cancer in women, and the second main cause of cancer death in women, after lung cancer.
Advances in screening and treatment have improved survival rates dramatically since 1989. There are around 3.1 million breast cancer survivors in the United States (U.S.). The chance of any woman dying from breast cancer is around 1 in 37, or 2.7 percent.
In 2017, around 252, 710 new diagnoses of breast cancer are expected in women, and around 40,610 women are likely to die from the disease.
Awareness of the symptoms and the need for screening are important ways of reducing the risk.
Breast cancer can affect men too, but this article will focus on breast cancer in women.
Contents of this article:
What is breast cancer?
Symptoms
10 risk factors
Diagnosis
Treatment
Prevention and outlook
Fast facts on breast cancer:
- Here are some key points about breast cancer. More detail is in the main article.
- Breast cancer is the most common cancer among women.
- Symptoms include a lump or thickening of the breast, and changes to the skin or the nipple.
- Risk factors can be genetic, but some lifestyle factors, such as alcohol intake, make it more likely to happen.
- A range of treatments is available, including surgery, radiation therapy, and chemotherapy.
- Many breast lumps are not cancerous, but any woman who is concerned about a lump or change should see a doctor.
What is breast cancer?
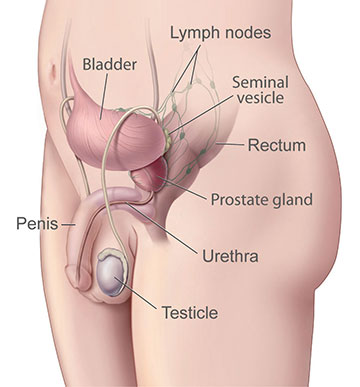
After puberty, a woman's breast consists of fat, connective tissue, and thousands of lobules, tiny glands that produce milk for breast-feeding. Tiny tubes, or ducts, carry the milk toward the nipple.
In cancer, the body's cells multiply uncontrollably. It is the excessive cell growth that causes cancer.
Breast cancer can be:
Ductal carcinoma: This begins in the milk duct and is the most common type.
Lobular carcinoma: This starts in the lobules.
Invasive breast cancer is when the cancer cells break out from inside the lobules or ducts and invade nearby tissue, increasing the chance of spreading to other parts of the body.
Non-invasive breast cancer is when the cancer is still inside its place of origin and has not broken out. However, these cells can eventually develop into invasive breast cancer.
Symptoms
The first symptoms of breast cancer are usually an area of thickened tissue in the breast, or a lump in the breast or in an armpit.
Other symptoms include:
a pain in the armpits or breast that does not change with the monthly cycle
pitting or redness of the skin of the breast, like the skin of an orange
a rash around or on one of the nipples
a discharge from a nipple, possibly containing blood
a sunken or inverted nipple
a change in the size or shape of the breast
peeling, flaking, or scaling of the skin on the breast or nipple
Most lumps are not cancerous, but women should have them checked by a health care professional.
10 risk factors
Breast cancer usually starts in the inner lining of milk ducts or the lobules that supply them with milk. From there, it can spread to other parts of the body.
The exact cause remains unclear, but some risk factors make it more likely. Some of these are preventable.
1. Age
The risk increases with age. At 20 years, the chance of developing breast cancer in the next decade is 0.6 percent. By the age of 70 years, this figure goes up to 3.84 percent.
2. Genetics
If a close relative has or has had, breast cancer, the risk is higher.
Women who carry the BRCA1 and BRCA2 genes have a higher risk of developing breast cancer, ovarian cancer or both. These genes can be inherited. TP53 is another gene that is linked to a greater breast cancer risk.
3. A history of breast cancer or breast lumps
Women who have had breast cancer before are more likely to have it again, compared with those who have no history of the disease.
Having some types of benign, or non-cancerous breast lumps increases the chance of developing cancer later on. Examples include atypical ductal hyperplasia or lobular carcinoma in situ.
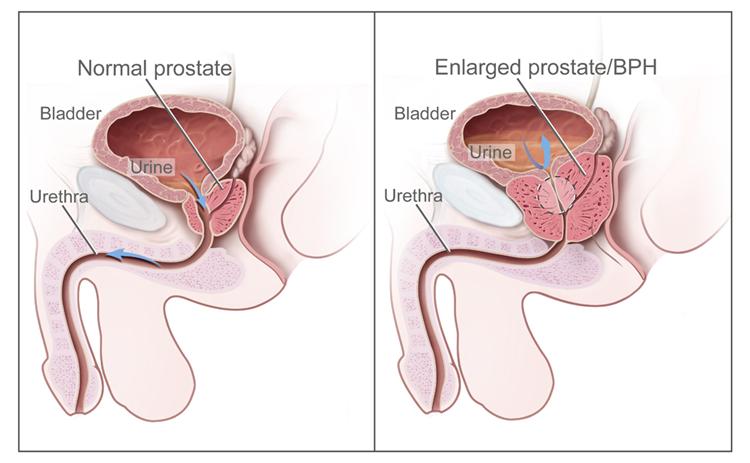
4. Dense breast tissue
Breast cancer is more likely to develop in higher density breast tissue.
5. Estrogen exposure and breast-feeding
Being exposed to estrogen for a longer period appears to increase the risk of breast cancer.
This could be due to starting periods earlier or entering menopause later than average. Between these times, estrogen levels are higher.
Breast-feeding, especially for over 1 year, appears to reduce the chance of developing breast cancer, possibly because pregnancy followed by breastfeeding reduces exposure to estrogen.
6. Body weight
Women who are overweight or have obesity after menopause may have a higher risk of developing breast cancer, possibly due to higher levels of estrogen. High sugar intake may also be a factor.
7. Alcohol consumption
A higher rate of regular alcohol consumption appears to play a role. Studies have shown that women who consume more than 3 drinks a day have a 1.5 times higher risk.
8. Radiation exposure
Undergoing radiation treatment for a cancer that is not breast cancer increases the risk of breast cancer later in life.
9. Hormone treatments
The use of hormone replacement therapy (HRT) and oral birth control pills have been linked to breast cancer, due to increased levels of estrogen.
10. Occupational hazards
In 2012, researchers concluded that exposure to certain carcinogens and endocrine disruptors, for example in the workplace, could be linked to breast cancer.
In 2007, scientists suggested that working night shifts could increase the risk of breast cancer, but more recent research concludes this is unlikely.
Cosmetic implants and breast cancer survival
Women with cosmetic breast implants who are diagnosed with breast cancer have a higher risk of dying from the disease and a 25 percent higher chance of being diagnosed at a later stage, compared with women without implants.
This could be due to due to the implants masking cancer during screening, or because the implants bring about changes in breast tissue. More research is needed.
Diagnosis
A diagnosis often occurs as the result of routine screening, or when a woman approaches her doctor after detecting symptoms.
Some diagnostic tests and procedures help to confirm a diagnosis.
Breast exam
The physician will check the patient's breasts for lumps and other symptoms.
The patient will be asked to sit or stand with her arms in different positions, such as above her head and by her sides.
Imaging tests
A mammogram is a type of x-ray commonly used for initial breast cancer screening. It produces images that can help detect any lumps or abnormalities.
A suspicious result can be followed up by further diagnosis. However, mammography sometimes shows up a suspicious area that is not cancer. This can lead to unnecessary stress and sometimes interventions.
An ultrasound scan can help differentiate between a solid mass or a fluid-filled cyst.
An MRI scan involves injecting a dye into the patient, so find out how far the cancer has spread.
Biopsy
A sample of tissue is surgically removed for laboratory analysis. This can show whether the cells are cancerous, and, if so, which type of cancer it is, including whether or not the cancer is hormone-sensitive.
Diagnosis also involves staging the cancer, to establish:
- the size of a tumor
- how far it has spread
- whether it is invasive or non-invasive
- whether it has metastasized, or spread to other parts of the body
- Staging will affect the chances of recovery and will help decide on the best treatment options.
Treatment
Treatment will depend on:
- Chemotherapy can be an option for breast cancer.
- Chemotherapy can be an option for breast cancer.
- the type of breast cancer
- the stage of the cancer
- sensitivity to hormones
- the patient's age, overall health, and preferences
The main options include:
- radiation therapy
- surgery
- biological therapy, or targeted drug therapy
- hormone therapy
- chemotherapy
- Factors affecting the choice will include the stage of the cancer, other medical conditions, and individual preference.
Surgery
If surgery is needed, the choice will depend on the diagnosis and the individual.
Lumpectomy: Removing the tumor and a small margin of healthy tissue around it can help prevent the spread of the cancer. This may be an option if the tumor is small and likely to be easy to separate from the surrounding tissue.
Mastectomy: Simple mastectomy involves removing the lobules, ducts, fatty tissue, nipple, areola, and some skin. Radical mastectomy removes muscle from the chest wall and the lymph nodes in the armpit as well.
Sentinel node biopsy: Removing one lymph node can stop the cancer spreading, because if breast cancer reaches a lymph node, it can spread further through the lymphatic system into other parts of the body.
Axillary lymph node dissection: If there are cancer cells on a node called the sentinel node, the surgeon may recommend removing several nymph nodes in the armpit to prevent the spread of disease.
Reconstruction: Following breast surgery, reconstruction can recreate the breast so that it looks similar to the other breast. This can be done at the same time as a mastectomy, or at a later date. The surgeon may use a breast implant, or tissue from another part of the patient's body.
Radiation therapy
Controlled doses of radiation are targeted at the tumor to destroy the cancer cells. Used from around a month after surgery, along with chemotherapy, it can kill any remaining cancer cells.
Each session lasts a few minutes, and the patient may need three to five sessions per week for 3 to 6 weeks, depending on the aim and the extent of the cancer.
The type of breast cancer will dictate what type of radiation therapy, if any, is most suitable.
Adverse effects include fatigue, lymphedema, darkening of the breast skin, and irritation of the breast skin.
Chemotherapy
Medications known as cytotoxic drugs may be used to kill cancer cells, if there is a high risk of recurrence or spread. This is called adjuvant chemotherapy.
If the tumor is large, chemotherapy may be administered before surgery to shrink the tumor and make its removal easier. This is called neo-adjuvant chemotherapy.
Chemotherapy can also treat cancer that has metastasized, or spread to other parts of the body, and it can reduce some symptoms, especially in the later stages.
It may be used to reduce estrogen production, as estrogen can encourage the growth of some breast cancers.
Adverse effects include nausea, vomiting, loss of appetite, fatigue, sore mouth, hair loss, and a slightly higher susceptibility to infections. Medications can help control many of these.
Hormone blocking therapy
Hormone blocking therapy is used to prevent recurrence in hormone-sensitive breast cancers. These are often referred to as estrogen receptive (ER) positive and progesterone receptor (PR) positive cancers.
Hormone blocking therapy is normally used after surgery, but it may sometimes be used beforehand to shrink the tumor.
It may be the only option for patients who cannot undergo surgery, chemotherapy, or radiotherapy.
The effects normally last for up to 5 years after surgery. The treatment will have no effect on cancers that are not sensitive to hormones.
Examples include:
- tamoxifen
- aromatase inhibitors
- ovarian ablation or suppression
- a luteinising hormone-releasing hormone agonist (LHRHa) drug called Goserelin, to suppress the ovaries
- Hormone treatment may affect a woman's future fertility.
Biological treatment
Targeted drugs destroy specific types of breast cancer. Examples include trastuzumab (Herceptin), lapatinib (Tykerb), and bevacizumab (Avastin). These drugs are all used for different purposes.
Treatments for breast and other cancers can have severe adverse effects.
The patient should discuss with a doctor the risks involved and ways to minimize the negative effects, when deciding on treatment.
Prevention and outlook
There is no sure way to prevent breast cancer, but some lifestyle decisions can significantly reduce the risk of breast and other types of cancer.
These include:
avoiding excess alcohol consumption
following a healthy diet with plenty of fresh fruit and vegetables
getting enough exercise
maintaining a healthy body mass index (BMI)
Women should think carefully about their options for breast-feeding and the use of HRT following menopause, as these can affect the risk.
Preventive surgery is an option for women at high risk.
Outlook
With treatment, a woman who receives a diagnosis of stage 0 or stage 1 breast cancer has an almost almost 100 percent chance of surviving for at least 5 years.
If the diagnosis is made at stage 4, the chance of surviving another 5 years is around 22 percent.
Regular checks and screening can help detect symptoms early. Women should discuss their options with a doctor.
.
Source:
http://www.medicalnewstoday.com/articles/37136.php